|
Case Report
A case of complete recovery from a transcranial bi-hemispheric civilian gunshot wound: A case report
1 General Surgery Resident, Howard University Hospital, 2041 Georgia Ave NW, Rm 4B16, Washington, DC, USA
2 Medical Student, Howard University College of Medicine, Howard University Hospital, 520 W St NW, Washington, DC, USA
3 Chief of Neurosurgery, Department of Surgery, Howard University Hospital, Washington, DC, USA
4 Professor of Surgery & Chief, Division of Trauma, Critical Care, and Surgical Nutrition, Department of Surgery, Howard University Hospital, Washington, DC, USA
Address correspondence to:
Hitesh Ramesh Reddy
General Surgery Resident, Howard University Hospital, 2041 Georgia Ave NW, Rm 4B16, Washington, DC 20060,
USA
Message to Corresponding Author
Article ID: 100092Z12HR2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Reddy HR, Bay COA, Layne SA, Williams M, Fossett D. A case of complete recovery from a transcranial bi-hemispheric civilian gunshot wound: A case report. J Case Rep Images Surg 2021;7:100092Z12HR2021.ABSTRACT
Introduction: Gunshot wounds have become one of the leading causes of traumatic brain injuries across the United States. Their incidence has been steadily increasing due in part to a surge in overall homicide rates and gang violence. The morbidity and mortality rate associated with a gunshot wound (GSW) to the head is high and this worsens with a transcranial GSW.
Case Report: Herein, we describe a case of a 25-year-old African-American male found down after he sustained GSW while driving his car. His initial Glasgow Coma Score (GCS) was 11 and was noted to have a facial laceration over the right eyebrow, later discovered to be a GSW on computed tomography evaluation of the head. It demonstrated a foreign body of metallic density that traversed both hemispheres of the brain and lodged itself in the left parietal region. Following appropriate medical and neurosurgical management, he made a complete recovery to his former neurological state in a span of four weeks.
Conclusion: Gunshot wounds to the head are associated with high morbidity and mortality in the civilian population. This case portrays rare survival and return to normal baseline function of a young male after sustaining a devastating bi-hemispheric injury to the the brain.
Keywords: Complete recovery from gunshot wound to the head, Non-operative management of a cranial GSW, Transcranial gunshot wound
Introduction
Gunshot wounds to the head in the civilian population have a high mortality rate. A missile whose trajectory crosses the midline structures of the brain and involves the ventricles, has about a 90% mortality rate; survivors usually have devastating morbidity. Our case describes a young male who survived a bi-hemispheric GSW to the head and recovered with no residual deficits from his injury with minimal surgical intervention.
Case Report
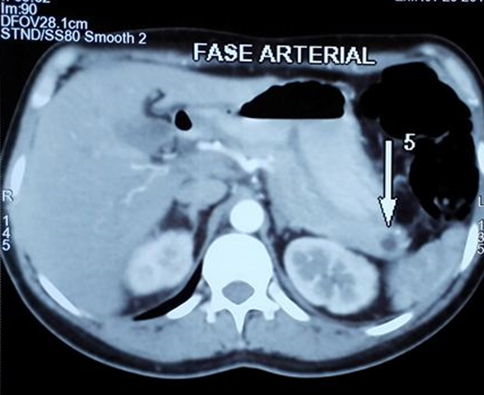
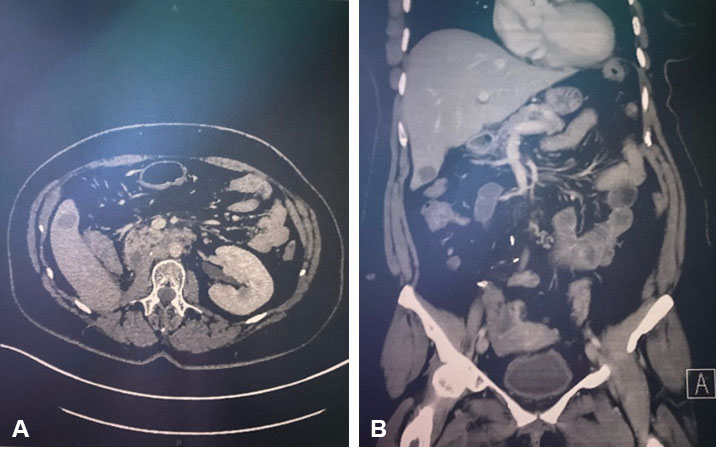
A 25-year-old African-American male was brought to Howard University Hospital as a trauma activation. The patient was described as being found with a facial laceration. At the scene, he was reported to be opening his eyes and moving all extremities when aroused. His car was noted to have multiple bullet holes in it. On primary survey, he was hemodynamically stable, his airway patent, breath sounds were clear bilaterally, and he had 2+ radial and dorsalis pedis pulses bilaterally. His GCS was 11; he was noted to be opening his eyes spontaneously, making incomprehensible sounds, and localizing to pain. On secondary survey, he had a 1 cm wound to the right supraorbital region with minimal bleeding. Other findings included vomitus around his mouth and decorticate posturing of his right upper extremity with normal movement of all other extremities. A non-contrast computed tomogram (CT) of the head demonstrated multiple hyperdense foreign bodies along a path from right to left involving the right supraorbital region, the right frontal lobe, and the left parietal lobe with involvement of the genu of the corpus callosum and left caudate. Scant blood was also noted in the lateral ventricular system and there were hemorrhagic changes in the left caudate nucleus as well as subarachnoid blood in the left sylvian fissure. A fracture of the inner and outer table of the skull with entry into the right frontal sinus was also identified as the bullet entry site.
Medical management
In the trauma bay, a fifty (50) gram bolus of mannitol, a prophylactic third (3rd) generation cephalosporin, and tetanus prophylaxis were given. A twenty (20%) mannitol drip infusing at 20 cc/h was continued for 36 hours after the bolus was given and seizure prophylaxis was initiated with levetiracetam. Upon transfer to the Surgical Intensive Care Unit, the patient was intubated due to concern for airway protection in anticipation of worsening cerebral edema which could lead to deterioration of his GCS.
Neurosurgical management
Due to the violation of the frontal sinus and cerebrospinal fluid visibly leaking from the gunshot entrance wound, the patient was taken to the operating room for craniotomy with dural repair. The depressed right frontal skull fracture was elevated, followed by exenteration of the frontal sinus, packing of the sinus with Gelfoam (Pfizer Inc., New York, NY USA) and dura was repaired with a pericranial patch graft. Bony fragments were removed and the surface of the brain irrigated and hemostasis assured. The craniotomy flap was re-affixed to the skull with a micro-plating system and the wound closed in a standard two-layered fashion.
On post-operative day (POD) #1, the patient was extubated. His GCS was 10 (E4 V1 M5) but with no movement of his right upper and lower extremity. He was unable to phonate though able to follow commands. On POD #2, he was transferred to the surgical floor with improved right upper and lower extremity motor function of 2/5. Progressively, through physical therapy, his right limb function improved over the course of the week. The lower extremity improved faster than the upper extremity. The patient remained able to follow commands, perform activities of daily living, and was able to verbally answer “yes” and “no” appropriately to questions. He retained his calligraphic style and was able to write his full name as well as well-formed sentences. He was amnestic to the events leading up to his hospital presentation and first days of admission; however, the memories of his hospital stay and his family, among others, remained intact.
D.L. returned to our Emergency Department 18 days post-discharge with headaches. He had full motor function of all extremities and was able to hold a conversation with minimal pauses between words. A CT scan of the head done revealed no interval changes compared to the post-operative scan. He was discharged home on oral analgesics and scheduled for a follow-up with the neurosurgeon. Over two subsequent follow-up visits at two and four weeks post-operatively, the patient had completely returned to normal neurologic and normal speech function. He remains on levetiracetam.
Discussion
Cranial GSWs are considered to be high-mortality, traumatic emergencies that surgical teams may elect to treat conservatively or aggressively based on the prognosis of injuries [1],[2]. Addressing the appropriate factors has been a topic of focus for many researchers [2],[3],[4],[5],[6] with guidelines around penetrating brain trauma, analyzing characteristics such as intracranial path and location, caliber and energy of bullet, changes in intracranial pressure and secondary bone fragments. These and other factors can be further associated with improved health outcomes or increased patient mortality depending on the physiology of the individual post-GSW.
Bi-hemispheric, transhemispheric, and transcranial GSWs have been well documented as negative indicators for survival with bi-hemispheric injury demonstrating the highest futility in medical and/or surgical management [7]. Seminal studies like Grahm et al. reported bi-hemispheric and transventricular penetration being associated with 90% mortality, while 10% of patients were classified as neurologically devastated [3],[4],[7],[8],[9],[10],[11]. Important to consider in this classification is the trajectory subclass: tangential, careening, ricocheting, penetrating, or perforating [11],[12]. A penetrating bullet that does not perforate allows for bullet trajectory to transfer energy through brain tissue, rather than carrying it through its exit out the opposite side. Following initial presentation, Kim et al. found that in addition to trajectory subclass, GCS is a significant, accurate prognostic factor to recognize as a significant factor in the treatment algorithm [7]. In activating the Advanced Trauma Life Support (ATLS) protocol, attention is paid to the presenting GCS, along with continual monitoring of vitals as necessary to limit intracranial hypertension, secondary to hemorrhage and edema. Patient mortality is also associated with abnormal pupillary response, specifically bilaterally fixed and dilated pupils during the patient’s treatment course. These patients are 67 times more likely to die as compared to patients with bilaterally reactive pupils, due to their direct tie to brain stem function [2],[7],[9],[10],[11]. Additional factors associated with higher mortality include advanced age, suicide attempt from close range, and occipital entry wound [11],[12].
We must consider the positive end of the patient outcome spectrum post-cranial GSW. The idea of patient functionality post-cranial GSW and their ability to maintain independent function has been associated with GCS>5, positive pupil reactivity, and unihemispheric or a bifrontal lobe bullet trajectory [3],[4]. Gressot et al. and Anderson et al. both advocate for the consideration of the patient’s complete presenting profile, as well as specific functionality goal points to help inform aggressive or conservative treatment options [3],[4]. These are institution-directed treatment philosophies which reject the notion that a singular factor such as a low GCS is a sufficient or complete measure of patient prognosis. In comparison, Howard University Hospital Level I Trauma Center’s protocols are in alignment with Advanced Trauma Life Support (ATLS) guidelines and brain trauma foundation guidelines of managing Traumatic Brain Injury (TBI) to consider the pathophysiology and its evolution over time not just the initial presentation as a prognostic marker. Initial non-operative management dictated by this patient’s physiology followed by neurosurgical elevation of the fractured frontal bone and frontal sinus repair as a non-emergent procedure might have aided this patient’s quick recovery to near baseline.
Conclusion
Bi-hemispheric gunshot wounds cause significant morbidity and mortality. Based on class III and IV evidence and respective studies, various scoring systems have been developed to prognosticate mortality. Although the index patient’s mortality was about 50% based on his bi-hemispheric trajectory of the bullet, he not only survived the initial traumatic injury but also made a complete recovery within a span of four weeks with very conservative management. Therefore, it may be clinically supportive to consider more than a single measure of patient prognosis before determining treatment options.
REFERENCES
1.
Stoffel M, Hüser N, Kayser K, et al. Cerebral gunshot wounds: A score based on three clinical parameters to predict the risk of early mortality. ANZ J Surg 2009:79(11):789–93. [CrossRef]
[Pubmed]

2.
Aarabi B, Tofighi B, Kufera JA, et al. Predictors of outcome in civilian gunshot wounds to the head. J Neurosurg 2014120(5):1138–46. [CrossRef]
[Pubmed]

3.
Gressot LV, Chamoun RB, Patel AJ, et al. Predictors of outcome in civilians with gunshot wounds to the head upon presentation. J Neurosurg 2014;121(3):645–52. [CrossRef]
[Pubmed]

4.
Anderson E, Kryzanski J. Prognosis and futility in neurosurgical emergencies: A review. Clin Neurol Neurosurg 2020;195:105851. [CrossRef]
[Pubmed]

5.
Kazim SF, Shamim MS, Tahir MZ, Enam SA, Waheed S. Management of penetrating brain injury. J Emerg Trauma Shock 2011;4(3):395–402. [CrossRef]
[Pubmed]

6.
7.
Kim LH, Quon JL, Cage TA, Lee MB, Pham L, Singh H. Mortality prediction and long-term outcomes for civilian cerebral gunshot wounds: A decision-tree algorithm based on a single trauma center. J Clin Neurosci 2020;75:71–9. [CrossRef]
[Pubmed]

8.
Grahm TW, Williams FC Jr, Harrington T, Spetzler RF. Civilian gunshot wounds to the head. Neurosurgery 1990;27(5):696–700. [CrossRef]
[Pubmed]

9.
?çer M, Zengin Y, Dursun R, et al. Factors affecting dural penetration and prognosis in patients admitted to emergency department with cranial gunshot wound. Eur J Trauma Emerg Surg 2015;43(5):611–5. [CrossRef]
[Pubmed]

10.
Turco L, Cornell DL, Phillips B. Penetrating bihemispheric traumatic brain injury: A collective review of gunshot wounds to the head. World Neurosurgery 2017;104:653–9. [CrossRef]
[Pubmed]

11.
Maragkos GA, Papavassiliou E, Stippler M, et al. Civilian gunshot wounds to the head: Prognostic factors affecting mortality: Meta-analysis of 1774 patients. Journal of Neurotrauma, 2017;35(22):2605–14. [CrossRef]
[Pubmed]

12.
Vakil MT, Singh AK. A review of penetrating brain trauma: Epidemiology, pathophysiology, imaging assessment, complications, and treatment. Emerg Radiol 2017;24(3):301–9. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Hitesh Ramesh Reddy - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Charles OA Bay - Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sylvonne A Layne - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mallory Williams - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Damirez Fossett - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Hitesh R Reddy et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.