|
Clinical Image
Heterotopic pancreatic tissue on the gallbladder wall: An incidental finding at laparoscopic appendectomy
1 Acute Surgical Unit, The Canberra Hospital, Yamba Drive, Garran, ACT 2605, Australia
2 General Surgery, Calvary Public Hospital, 5 Mary Potter Circuit, Bruce, ACT 2617, Australia
Address correspondence to:
Natalie Quarmby
Acute Surgical Unit, The Canberra Hospital, Yamba Drive, Garran, ACT 2605,
Australia
Message to Corresponding Author
Article ID: 100104Z12NQ2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Quarmby N, Rodrigues AN, Varley M, Beenen E. Heterotopic pancreatic tissue on the gallbladder wall: An incidental finding at laparoscopic appendectomy. J Case Rep Images Surg 2022;8(2):1–3.ABSTRACT
No Abstract
Keywords: Appendectomy, Cholecystectomy, Heterotopic pancreas
Case Report
A 21-year-old male with a known background history of asthma, depression, and obstructive sleep apnea presented with a typical history of acute appendicitis comprising three days of generalized abdominal pain migrating to the right iliac fossa, associated with loose stools. On examination he had peritonism in the right iliac fossa. His inflammatory markers were mildly raised; all other pathology results including liver function tests and lipase level were within normal limits. A computed tomography (CT) scan and ultrasound ordered by the general practitioner (GP) prior to presentation were consistent with acute appendicitis. No other abnormalities were reported.
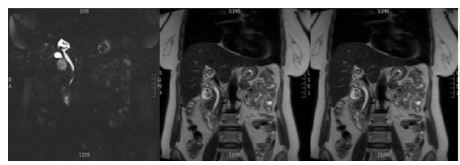
The patient was admitted under the care of the Acute Surgical Unit and was commenced on triple antibiotic therapy using Ampicillin, Metronidazole, and Gentamicin. He underwent a laparoscopic appendectomy on day one of admission, and during inspection of the peritoneal cavity, an exophytic polypoid lesion on the external wall of the gallbladder was seen (Figure 1). Intraoperative consultation was sought from an upper gastrointestinal surgeon, and the decision was made to not biopsy the lesion at the time of surgery due to its unknown extent within the gallbladder wall, plus the desire to avoid spillage of potentially malignant cells into the peritoneal cavity. The appendectomy was completed and the post-operative course was uncomplicated with the patient being discharged on post-operative day one. Although the polypoid lesion did have a macroscopically benign appearance (smooth, no adherence, no obvious infiltration of surrounding tissues), during outpatient follow-up it was decided with the patient to perform a cholecystectomy to achieve a complete excisional biopsy and obtain a definitive diagnosis. An uncomplicated laparoscopic cholecystectomy was performed. Histopathology demonstrated an intact gallbladder with an exophytic nodule at the gallbladder fundus measuring 10 × 6 × 5 mm in size. Sections from the nodule at the gallbladder fundus identified pancreatic heterotopia with presence of acinar cells and ductal structures (Figure 2). The lining of the gallbladder demonstrated adenomyomatosis, but no other abnormalities.
Discussion
Originally described by Jean Schultz et al. in the 18th century, and later histologically confirmed in 1859 by Klob, heterotopic or ectopic pancreas is the presence of congenital pancreatic tissue in a location that is anatomically unrelated to the pancreas [1],[2]. Previous autopsy studies estimated the frequency of heterotopic pancreas tissue anywhere along the gastrointestinal (GI) tract between 0.5% and 13.7%, and it has been described in 2% of laparotomies [2],[3]. Typical locations of heterotopic pancreas include the stomach, small intestine, and spleen. More rarely ectopic pancreas tissue can be found in other locations including the gallbladder and lungs [4]. In a systematic review published in 2021, Aborajooh et al. reported a total of 38 cases from 1959 to 2020 of heterotopic pancreatic tissue in the gallbladder, representing approximately 1–2% of all cases of heterotopic pancreas [5]. Most cases were incidental diagnosis during cholecystectomies for symptomatic gallstone disease leading to an increased finding in women and an age above 40 [4],[5]. In approximately 10% of cases the tissue was thought to resemble gallbladder polyps or malignancy on imaging, often found as a submucosal lesion up to 3 cm with an endoluminal growth pattern, which formed the indication for surgery [2],[5].
The Heinrich classification from 1909 was updated by Fuentes in 1973 to include four types according to its constitutional components, with Type I—tissue consists of all components of normal pancreatic tissue, including acini, ducts, and islet cells; Type II—tissue consists of ducts only; Type III—tissue consists of acini only (exocrine); and Type IV—tissue consists of islet cells only (endocrine) [1],[2],[6].
Studies indicate that the contrast enhancement characteristics and homogeneity of the tissue correlates well with its histological composition. Lesions with enhancement that is greater than or equal to that of the pancreas are dominated by acini, while lesions with less enhancement tend to be dominated by ducts and hypertrophied muscle [6],[7].
There are several theories regarding the development of heterotopic pancreas, with the most widely held theories being the “misplacement theory,” wherein deposits of pancreatic tissue are “dropped” into the developing gastrointestinal system, which accounts for the typical findings of heterotopic pancreatic tissue in the derivatives of the primitive foregut [6]. Alternatively, it may be considered the result of early separation of the pancreas during rotation of the GI tract [1],[8]. The heterotopic pancreas tissue may be affected by the same pathological conditions as the pancreas itself including pancreatitis, pseudocyst formation, and malignancy [1],[4]. Elevation of pancreatic enzymes during inflammation is very mild due to the small volume of inflamed tissue affected and the tissue may enhance less avidly when acutely inflamed [6].
Conclusion
Although rare, heterotopic tissue should be considered as part of differential diagnosis for unexplained abdominal pain, bleeding from the GI tract or weight loss, and may be considered as a cause for acute idiopathic pancreatitis. When found in the asymptomatic patient, careful consideration should be given as to the risks of malignant transformation or chronic pancreatitis against the surgical risks involved, and when intervention is deemed necessary, minimally invasive procedures should be considered.
REFERENCES
1.
Inoue Y, Hayashi M, Arisaka Y, Higuchi K, Egashira Y, Tanigawa N. Adenocarcinoma arising in heterotopic pancreas (Heinrich type III): A case report. J Med Case Rep 2010;4:39. [CrossRef]
[Pubmed]

2.
Sanchiz Cárdenas EM, Soler Humanes R, Lavado Fernández AI, Díaz Nieto R, Suárez Muñoz MA. Ectopic pancreas in gallbladder. Clinical significance, diagnostic and therapeutic implications. Rev Esp Enferm Dig 2015;107(11):701–3. [CrossRef]
[Pubmed]

3.
Sroczyński M, Sebastian M, Hałoń A, Rudnicki J, Sebastian A, Kumar Agrawal AK, Piekarz P. Pancreatic heterotopic in the gallbladder: An incidental finding after cholecystectomy. Folia Histochem Cytobiol 2013;51(2):174–7. [CrossRef]
[Pubmed]

4.
Sharma SP, Sohail SK, Makkawi S, Abdalla E. Heterotopic pancreatic tissue in the gallbladder. Saudi Med J 2018;39(8):834–7. [CrossRef]
[Pubmed]

5.
Aborajooh E, Ghayada IKK, Lafi YMI. Heterotopic pancreas in the gallbladder: Case report and literature review. Case Rep Med 2021;2021:6611291. [CrossRef]
[Pubmed]

6.
Rezvani M, Menias C, Sandrasegaran K, Olpin JD, Elsayes KM, Shaaban AM. Heterotopic pancreas: Histopathological features, imaging findings, and complications. Radiographics 2017;37(2):484–99. [CrossRef]
[Pubmed]

7.
Kim DW, Kim JH, Park SH, et al. Heterotopic pancreas of the jejunim: Association between CT and pathology features. Abdom Imaging 2015;40(1):38–45. [CrossRef]
[Pubmed]

8.
Al-Shraim M, Rabie ME, Elhakeem H, Kandeel A, Shah MT, Jamil S. Pancreatic heterotopia in the gallbladder associated with chronic cholecystitis: A rare combination. JOP 2010;11(5):464–6.
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Natalie Quarmby - Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Andrea Nicole Rodrigues - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Martin Varley - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Edwin Beenen - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Natalie Quarmby et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.