|
Case Report
Hereditary hemorrhagic telangiectasia with bilateral pulmonary vascular malformations and a cerebral abscess as a complication: A case report
1 MD, PhD student, Clinical Department of Diagnostic and Interventional Radiology, University Hospital Centre Osijek, Faculty of Medicine, Josip Juraj Strossmayer University of Osijek, Osijek, Croatia
2 Associate Professor, Department of Hematology, Clinic of Internal Medicine, University Hospital Centre Osijek, Faculty of Medicine, Josip Juraj Strossmayer University of Osijek, Osijek, Croatia
3 Medical student, Faculty of Medicine, Josip Juraj Strossmayer University of Osijek, Osijek, Croatia
4 Associate Professor, Health Centre Osijek, Faculty of Medicine, Josip Juraj Strossmayer University of Osijek, Osijek, Croatia
5 MD, PhD, Clinic of Paediatrics, University Hospital Centre Osijek, Croatia; Faculty of Medicine, Josip Juraj Strossmayer University of Osijek, Osijek, Croatia
6 MD, PhD, Department of Neurosurgery, University Hospital Centre Osijek, Faculty of Medicine, Josip Juraj Strossmayer University of Osijek, Osijek, Croatia
Address correspondence to:
Zdravka Krivdić Dupan
Clinical Department of Diagnostic and Interventional Radiology, University Hospital Centre Osijek, J. Huttlera 4, Osijek,
Croatia
Message to Corresponding Author
Article ID: 100105Z12ZD2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Dupan ZK, Periša V, Guljaš S, Laslo D, Salha T, Tomac V, Koruga N. Hereditary hemorrhagic telangiectasia with bilateral pulmonary vascular malformations and a cerebral abscess as a complication: A case report. J Case Rep Images Surg 2022;8(1):4–8.ABSTRACT
Introduction: Hereditary hemorrhagic telangiectasia (HHT) also known as Osler–Weber–Rendu syndrome is a relatively common, under-recognized autosomal-dominant disorder that results from multisystem vascular dysplasia. It is characterized by telangiectasis and arteriovenous malformations of skin, mucosa, and viscera.
Case Report: A 26-year-old man presented with an 8-day history of headache, fever, cough, right hemiparesis, motor dysphasia, and dysgraphia. The urgent brain computed tomography (CT) scan revealed a bulky rounded left frontal lobe lesion, with peripheral contrast enhancement and marked perilesional edema, indicating a brain abscess or metastasis. A brain magnetic resonance imaging showed an intra-axial hypovascular round enhancing left frontal lobe lesion, with pronounced perilesional edema. Laboratory findings discovered severe polycythemia with normal level of erythropoietin and gas analysis of blood revealed hypoxemia of secondary cause. Computed tomography of the lungs suggested pulmonary arteriovenous malformations (AVMs) in the right and left lung. Contrast-enhanced chest CT scan confirmed AVM of the lungs, while abdominal CT scan ruled out AVM of the liver. The brain abscess was treated neurosurgically. The patient reported positive family history of epistaxis.
Conclusion: Brain abscess may be the first manifestation of HHT and early clinical recognition of HHT in patients with positive family history of epistaxis may help to prevent complications.
Keywords: Arteriovenous malformations, Brain abscess, Hereditary hemorrhagic telangiectasia, Hypoxemia, Polycythemia
Introduction
Hereditary hemorrhagic telangiectasia (HHT) or Rendu–Osler–Weber syndrome is an autosomal-dominantly inherited vascular disease that occurs in at least 1 in 10,000 individuals [1]. Hereditary hemorrhagic telangiectasia is genetically heterogenous disease caused by mutations of genes which encodes proteins important in transforming growth factor beta (TGF-b) signaling pathway. Three major genes are the most commonly affect by mutations. Mutation of endoglin (ENG) and activin A receptor type II-like 1 (ACVRL1/ALK1) causes HHT1 and HHT2 disease type. Mutation in gene SMAD4 causes a combined juvenile polyposis/HHT (JP/HHT) syndrome. In all three cases, mutation causes hypoproduction of gene product and thus abnormal angiogenesis [2]. Abnormal angiogenesis causes small vascular lesions of skin and mucosa especially of the oral and nasal cavity, lips, fingers, and upper gastrointestinal tract. Larger vascular lesions configuring arteriovenous malformations (AVMs) are congenital structural changes of blood vessels with high blood flow. Those are clinically important because they usually exist in vital organs such as brain, liver, and lungs. Cerebral AVMs can cause intracranial hemorrhage in infants and children that can be life-threating condition [3]. Three criteria must be fulfilled for diagnosis of HHT, those are mucocutaneous telangiectasis, AVMs of lung, brain, or liver and positive family history of those abnormalities [1]. The most common clinical presentation of HHT is epistaxis, it is reported in about 95% of individuals with HHT during life, but only in 50% of individuals before age of 10. It is recommended to start treatment of HHT in the first six months of life, but diagnosis, usually, cannot be set based on clinical presentation during the first year of life, therefore genetic testing and molecular diagnostics are the key to set early diagnosis and start treatment during the first six months of a patient’s life [3].
Case Report
The patient was a 26-year-old Caucasian man who presented with an 8-day history of headache, fever, cough, right hemiparesis, motor dysphasia, and dysgraphia. He had no remarkable medical history except hypothyroidism. On initial physical examination the patient had a body temperature of 36,8 °C and a blood pressure of 125/78 mmHg. Laboratory findings discovered severe polycythemia. Significant findings included hemoglobin 184 g/L, hematocrit of 0.54, and red blood cell count of 6.35 × 10 12/L. Other laboratory findings were normal. The urgent brain computed tomography (CT) scan revealed a bulky rounded left frontal lobe lesion, measuring 4.9×3.6×4.4 cm (AP, LL, CC), with peripheral contrast enhancement and marked perilesional edema, indicating a brain abscess or metastasis (Figure 1A and Figure 1B).
A brain magnetic resonance imaging (MRI) showed an intra-axial hypovascular round enhancing left frontal lobe lesion, with pronounced perilesional edema, contralateral ventricular displacement, and subfalcine herniation, measured 4.9×3.7×4.3 cm (AP, LL, CC) in maximum transverse dimensions.
High signal intensity on diffusion weighted imaging (DWI) and corresponding reduced apparent diffusion coefficient (ADC) indicates a brain abscess (Figure 2).
The patient was surgically treated under general anesthesia. The left-sided craniotomy and C-shaped durotomy were performed. Abscess was verified under ultrasound guidance and punctured with the Cushing needle. Around 60 mL of pus were evacuated and prepared for microbiological testing. The abscess capsule was completely removed in microsurgical technique and meticulous hemostasis was obtained. Dural closure, cranioplasty, and the wound closure were performed in a regular fashion.
An adequate antibiotic treatment was applied during an early follow-up. The patient was examined preoperatively by an infectologist who introduced antimicrobial therapy (meropenem 3×2 g and vancomycin 2×1 g administered intravenous (IV)).
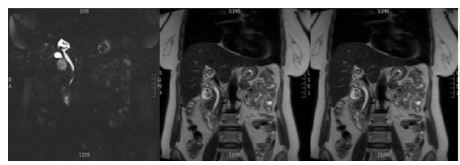
Preoperative symptoms completely resolved. Follow-up head CT scan revealed complete removal of abscess. Because of polycythemia the patient was referred to a hematologist. Gas analysis of blood was performed, and we determined hypoxemia which was indicative for the secondary cause of polycythemia. Level of erythropoietin was normal (16.45 mIU/mL). Because of hypoxemia and fatigue with physical exertion (pH 7.45, pCO2 3.98, pO2 5.83, HCO3 20.6, SO2 82.2%). Pulmonological examination was preferred, and computed tomography (CT) was proposed. Computed tomography of the lungs suggested pulmonary AVMs in the right and left lung, preferably in basal segments (Figure 3). Contrast-enhanced chest CT scan confirmed AVM of the lungs, while abdominal CT scan showed no evidence of AVM of the liver. 1.5 years after neurosurgical treatment of a brain abscess, a suspected diagnosis of HHT was made. He had a positive family history of epistaxis (father and grandfather). The patient rejected the transcatheter embolization of pulmonary AVMs.
Discussion
One of the most serious potential complications of HHT is brain abscess which has a high mortality. An abscess results from various conditions like a spread from sinus or ear infection, trauma, or due to hematogenous infection paradoxical emboli due to right to left shunt or bacterial spreading of an ischemic portion of the brain after paradoxical sterile emboli [4],[5]. Approximately 1–10% of patients with HHT develop brain abscess. The risk is higher in patients with pulmonary AVMs. Pulmonary AVMs are typically asymptomatic and usually the first presentation are serious neurological complications such as cerebrovascular event or abscess [4],[6],[7]. Pulmonary AVMs are vascular malformations without a capillary network which enables direct communication between the pulmonary artery and extra cardiac right to left shunt. Approximately 80–95% of pulmonary AVMs are associated with hereditary hemorrhagic telangiectasia [8].
Before 1977, surgery was the only method of treatment for pulmonary arteriovenous malformations. As the most common clinical presentations are recurrent epistaxis and hemoptysis, surgical resection was the best curative treatment to prevent future episodes and recurrence of hemoptysis. Procedures performed included ligation, excision, lobectomy, segmentectomy, and pneumonectomy. As a mode of treatment, it carries the same risks as any thoracic surgery. However, older studies reflect no perioperative mortality in patients undergoing resection of the pulmonary AVMs. The decreased mortality in newer studies reflects the advances in surgical technique which are employed in contemporary procedures.
Embolization treatment is a procedure in which the feeding arteries to a pulmonary AVM are occluded. Endovascular therapy of this type is an outpatient-based procedure with minimal invasiveness. The method involves localization of the pulmonary AVM by angiography after which a catheter is inserted, and either a coil or inflatable balloon is released to impede the communication. Periprocedural mortality has not been reported with this technique, and the most common complication is pleuritic chest pain, which resolves on its own. With a success rate of 98.7%, this is the preferred method of treatment for most patients. Thus, it is claimed that percutaneous embolization is an efficient, safe, and sustained therapy for pulmonary AVMs [9].
All reported cases of brain abscess in HHT are associated with PAVMs [10],[11]. Because a previous study indicated that patients with brain abscess and HHT have higher mortality around 40% compared to 10–15% in patients with brain abscess without HHT it is important to recognize the underlying cause [4],[7].
Conclusion
Brain abscess may be the first manifestation of hereditary hemorrhagic telangiectasia with a potentially fatal outcome. Early clinical recognition of HHT is important because screening in these patients and affected family members may help prevent complications.
REFERENCES
1.
McDonald J, Wooderchak-Donahue W, VanSant Webb C, Whitehead K, Stevenson DA, Bayrak-Toydemir P. Hereditary hemorrhagic telangiectasia: Genetics and molecular diagnostics in a new era. Front Genet 2015;6:1. [CrossRef]
[Pubmed]

2.
Faughnan ME, Mager JJ, Hetts SW, et al. Second International guidelines for the diagnosis and management of hereditary hemorrhagic telangiectasia. Ann Intern Med 2020;173(12):989–1001. [CrossRef]
[Pubmed]

3.
McDonald J, Bayrak-Toydemir P, DeMille D, Wooderchak-Donahue W, Whitehead K. Curaçao diagnostic criteria for hereditary hemorrhagic telangiectasia is highly predictive of a pathogenic variant in ENG or ACVRL1 (HHT1 and HHT2). Genet Med 2020;22(7):1201–5. [CrossRef]
[Pubmed]

4.
Dong SL, Reynolds SF, Steiner IP. Brain abscess in patients with hereditary hemorrhagic telangiectasia: Case report and literature review. J Emerg Med 2001;20(3):247–51. [CrossRef]
[Pubmed]

5.
Nam TK, Park YS, Kwon JT. Brain abscesses associated with asymptomatic pulmonary arteriovenous fistulas. J Korean Neurosurg Soc 2017;60(1):118–24. [CrossRef]
[Pubmed]

6.
Hall WA. Hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber disease) presenting with polymicrobial brain abscess. Case report. J Neurosurg 1994;81(2):294–6. [CrossRef]
[Pubmed]

7.
Themistocleous M, Giakoumettis D, Mitsios A, Anagnostopoulos C, Kalyvas A, Koutsarnakis C. Hereditary hemorrhagic telangiectasia patient presenting with brain abscess due to silent pulmonary arteriovenous malformation. Pan Afr Med J 2016;25:145. [CrossRef]
[Pubmed]

8.
Cartin-Ceba R, Swanson KL, Krowka MJ. Pulmonary arteriovenous malformations. Chest 2013;144(3):1033–44. [CrossRef]
[Pubmed]

9.
Martinez-Pitre PJ, Khan YS. Pulmonary Arteriovenous Malformation (AVMs). 2022 Jun 27. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.
[Pubmed]

10.
White RI Jr, Lynch-Nyhan A, Terry P, et al. Pulmonary arteriovenous malformations: Techniques and long-term outcome of embolotherapy. Radiology 1988;169(3):663–9. [CrossRef]
[Pubmed]

11.
Dyer NH. Cerebral abscess in hereditary haemorrhagic telangiectasia: Report of two cases in a family. J Neurol Neurosurg Psychiatry 1967;30(6):563–7. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Zdravka Krivdić Dupan - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Vlatka Periša - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Silva Guljaš - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Dorian Laslo - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Tamer Salha - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Višnja Tomac - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Nenad Koruga - Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Zdravka Krivdić Dupan et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.